ANTI-VIRAL DRUGS
and
COVID-19
Anti-viral drugs may prove to be one of the answers (in conjunction with vaccines, booster shots, and antibody treatments, such as monoclonal antibody therapies) to how to live ‘normally’ alongside SARS-CoV-2, a virus which may be with us in one form or another for some time to come. (Information as of January 2022).
HOW VIRUSES WORK
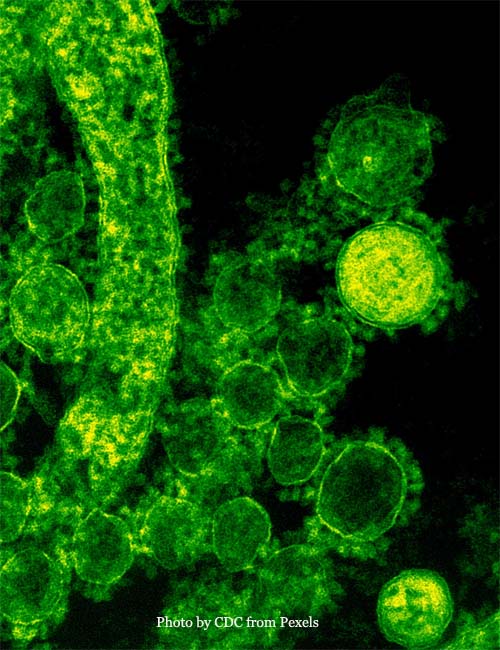
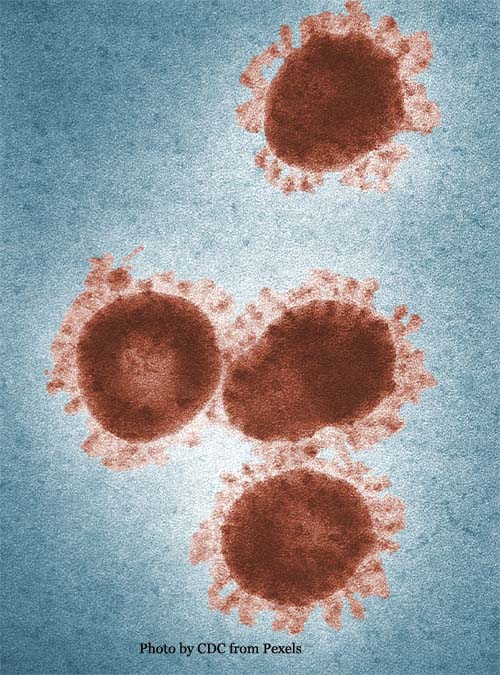
In order to live, a virus must replicate itself by copying its genetic code or blueprint, a molecule of ribonucleic acid or ‘RNA.’ If a virus can enter a cell and hijack that cell’s reproductive machinery and replicate itself, the host cell will then be forced to release those replications and wreak havoc throughout the body.
HOW VACCINES WORK
We now have vaccines available that generate proteins called antibodies that can recognize a virus and inactivate it before it can enter the body’s cells and cause an infection.
But it is the nature of a virus to mutate and if it has mutated enough to get past the antibodies and has successfully entered cells, infections in the unvaccinated and ‘breakthrough’ infections of vaccinated individuals can occur and specialized treatments of the infection become necessary.
TREATMENTS FOR
COVID-19 INFECTIONS
Monoclonal Antibody Therapies
Monoclonal antibodies are antibodies that are selected for their strong ability to resist a virus. When they enter the body, they look for and attach to the spike protein that sticks out of the coronavirus that causes COVID-19. When they attach to the spike protein, they can block the virus’s ability to enter cells and slow down the infection. In 2020, the FDA issued an emergency use authorization of monoclonal antibodies as a treatment option for COVID-19.
Monoclonal antibody therapies, which are typically delivered via an IV infusion, have become a major treatment used for non-hospitalized COVID-19 patients.
Anti-Viral Drugs
Replication of a virus can be prevented if the molecular structure of its RNA is disturbed so it cannot replicate and force a host cell to obey its commands. This is what researchers in molecular biology have been working tirelessly on to get us out from under the clutches of COVID-19. Anti-viral drugs are the result of this continuing research.
Remdesivir – the First Approved Anti-Viral Drug for COVID-19
Remdesivir was the first antiviral approved for Sars-CoV-2 infection and was initially developed for the treatment of Ebola. Without getting too technical, the drug mimics one of the building blocks of RNA and can get incorporated into a virus’ RNA. This altered RNA cannot send out the proper instructions it needs to start putting together its own RNA. The result is a dysfunctional RNA and the newly developing virus withers away.
Unfortunately,
Remdesivir must be given intravenously once symptoms have occurred and this is
usually in a hospital setting. An oral antiviral drug that does not require
hospitalization is obviously preferable.
Oral Anti-Viral Drugs - Pills
Paxlovid
Paxlovid is an oral anti-viral drug developed by Pfizer. This drug is a protease inhibitor (which inactivates an enzyme known as a protease).
A virus synthesizes large proteins based on instructions from its RNA. These larger proteins are then broken down by protease enzymes into the smaller proteins that the virus needs to invade a cell and replicate. The anti-viral pill, Paxlovid, interferes with this breakdown process.
Paxlovid is combined with a drug called Ritonavir (that interferes with the activity of an enzyme that would normally degrade it). When given within three days of the appearance of the first symptoms, it has been shown to cut the risk of hospitalization and death by 89 percent for adults with COVID-19 at high risk of developing severe disease.
As of December 21, 2021, Paxlovid has been authorized by the FDA for people 12 years of age and older who are at a high risk of getting seriously ill if they contract the virus.
Molnupiravir (Lagevrio)
A second COVID-19 oral anti-viral drug, Molnupiravir, developed by Merck, works much like Remdesivir. It is a nucleoside, a type of antiviral that intentionally inserts errors into the copying process of a virus.
Unlike Remdesivir, Molnupiravir does not stop new RNA from being formed but the shape of the entire RNA molecule is changed instead and the new versions of the RNA of the virus are ‘mutants. When enough of these mutations occur in a virus’ RNA, it cannot send out the proper instructions for multiplication.
As of December 22, 2021, Molnupiravir has been authorized for use in high-risk people 18 or older who have been diagnosed with COVID-19. It appears less effective than Paxlovid, since a large clinical trial found that it only reduced hospitalization and death from COVID-19 by 30 percent.
There is also a legitimate concern with this anti-viral drug. Since it obstructs viral replication, there is also the theoretical risk it could interact and mutate human cells. Although Merck has emphasized there is no evidence this could happen, it does have some scientists concerned. Thus, the FDA has said that given the potential risk to fetuses, Molnupiravir is not recommended for pregnant people.
ORAL ANTI-VIRAL DRUGS vs. OMICRON and
FUTURE VARIANTS of COVID-19
It is anticipated that the anti-viral pills will work equally well against the Omicron and future variants of the SARS-CoV-2 virus because the pills do not target the virus’ spike protein. This spike protein, as we know, is used by the virus to latch onto human cells. The spike protein is the primary target for most vaccines (and boosters) and antibody drugs, but the Omicron variant has more than 30 mutations on that spike protein rendering the monoclonal antibodies ineffective against this variant and allowing for the possibility of 'breakthrough' infections in vaccinated individuals as well.
Oral anti-viral pills are cheaper and easier to administer than monoclonal antibody treatments. However, because the treatment must be started within a few days of symptoms, it may be difficult for many people to get a COVID-19 test, a result, and then see a doctor for an oral anti-viral drug prescription in that window of time.
Nonetheless, oral anti-viral pills can be viewed as a significant tool in battling the virus in at-risk populations and eventually in lower-income countries where vaccines are not readily available.
GENERAL CONCERN ABOUT
ANTI-VIRAL DRUGS
The 2 oral drugs, Paxlovid and Molnupiravir (and others to follow) should have a great impact on the treatment of COVID-19 infections. Although they offer a treatment option that may reduce the severity of an infection, they are NOT substitutes for the use of vaccines that can PREVENT infections.
The vaccines we have now can be ‘tweaked’ to work with continued mutations of the coronavirus. Unfortunately, this may mean booster shots will have to administered on a regular basis, but these shots can certainly play an essential role in allowing the world to eventually return to some degree of normalcy.
There is some concern that the introduction of the new anti-viral drugs would give vaccine-hesitant persons the idea that infection is no big deal because it can be dealt with by a pill. Hopefully, though, the old adage that an ounce of prevention is worth a pound of cure will still prevail!
Top of Anti-Viral Drugs and COVID-19
"The Cleanest Clean You've Ever Seen."
by
ABC Oriental Rug & Carpet Cleaning Co.
130 Cecil Malone Drive Ithaca, NY 14850
607-272-1566